A new study on office-based treatment of adolescents with Suboxone was just published by the Journal of the American Society of Addiction Medicine.
The good news, drug screens were done at clinic visits and 85% of drug screens were negative for heroin and marijuana. (It’s not clear why they limited testing to these drugs.)
The bad news, most folks stopped coming to the clinic:
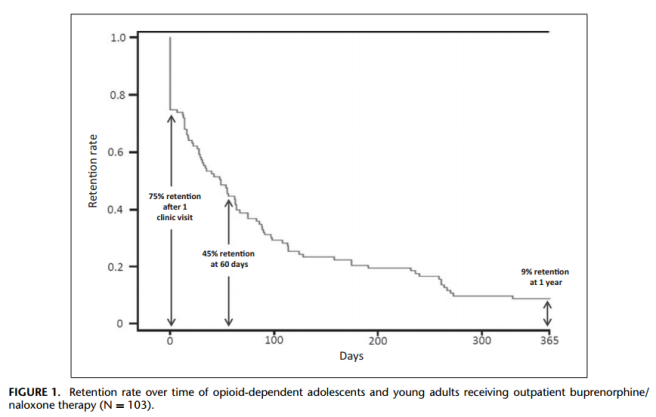
Program retention was the major barrier to treatment success (Fig. 1). After 1 visit, 75% returned for a second visit. At 60 days, 45% of patients were still retained, and by 1 year 9% were retained and still active in the program.
This means that, of the 103 young people in the study, 67 of them dropped out within 2 months and 94 dropped out within a year.
This would appear to undermine arguments for buprenorphine as a strategy for preventing overdose deaths.
These retention problems don’t stop the authors from putting a positive spin on it:
We submit these retention rates as preliminary benchmarks against which other approaches might be compared. Considering the chronic relapsing nature of addiction, long-term opioid substitution therapy with BUP/NAL should gain wider acceptance. Outpatient BUP/NAL should be seen as an important component of adolescent and young adult opioid addiction treatment.
Unfortunately, now that this is published, this spin will be used to frame this treatment as evidence-based.

When Titan puts out Probuphine this will be moot. What do you think the trajectory will be for these kids when doctors can implant them with the drug? http://www.titanpharm.com/press/2013/13-12-23-Titan-Minutes-FDA.htm
This had slipped by me. Wow.
This is a very poor retention rate. I’ve not read the paper but I suspect the age of the patients involved must be part of the issue. I appreciate your point though that even with these terrible results, a positive spin is inevitable.
We’ve had similar issues in Scotland in terms of ‘evidence based’ replacement therapy, mainly methadone. Until recently methadone was found in a majority of drug related deaths (more than heroin) with 60% of those dying of a drug death having methadone in their system despite never having been prescribed it – diversion of prescription methadone is a problem. Things are improving due to increased supervision (of methadone dosing – previously ampoules etc could be taken home), but aside from this methadone has other issues, such as being just as addictive as heroin, with its own stigma from the public and practitioners – methadone is usually taken at the chemist counter, without much privacy being provided. I think in many cases heroin addicts in Scotland are being weaned off of heroin only to be left with a state sponsored methadone habit. The big winners are big pharma.
http://www.sdf.org.uk/news-and-media/general-news/general-news-archive-2013/most-drug-deaths-in-scotland-are-users-not-in-treatment-says-new-report/
Again, I think that there is no one way fixes all recovery model. I know many long-term residential programs that use very deceiving designs to demonstrate effectiveness of their programs. Many programs only follow-up for a short time after folks complete the program and don’t count those who do not complete their program in the final numbers, which is misleading and skews the numbers. With that said, I know many folks who have been successful with medical detox tools as part of an overall plan for recovery. I also know many people who would never take the plunge and also have died because they were opiate users not willing to go through the tough love approach to recovery.